Espin TM Tablet 10's


MRP ₹133
(Inclusive of all Taxes)
₹19.9 Cashback (15%)
Know Your Delivery Time
Provide Delivery Location

Secure Payment

India's Most Trusted Pharmacy

Genuine Products
Composition :
Manufacturer/Marketer :
Consume Type :
Return Policy :
Expires on or after :
About Espin TM Tablet
Espin TM Tablet belongs to the class of medicines called ‘anti-hypertensive’ primarily used to treat hypertension (high blood pressure). Hypertension or high blood pressure is a chronic condition in which the blood's force against the artery wall is high. As a result, it leads to heart disease, irregular heartbeat and other complications.
Espin TM Tablet is a combination of two medicines include: S-Amlodipine and Telmisartan, which are antihypertensive medicines. S-amlodipine is a calcium channel blocker and works by relaxing and widening the blood vessels. It is equally efficacious at a half dose with better tolerability and fewer side effects, including peripheral oedema, than amlodipine. Telmisartan is an angiotensin II receptor antagonist that lowers blood pressure and increases blood flow by preventing blood vessel narrowing. It is used to lower the chances of stroke, heart attack and death. Altogether, Espin TM Tablet helps to lower high blood pressure, chest pain (angina) and other conditions caused by coronary artery disease.
Take Espin TM Tablet as prescribed by your doctor. You are advised to take Espin TM Tablet as long as your doctor has prescribed it for you, depending on your medical condition. In some cases, you may experience certain side effects, dizziness, stomach pain, nausea, constipation, double vision, muscle cramps, swollen ankles, oedema (fluid retention), and hypotension (low blood pressure). Most of these side effects of Espin TM Tablet do not require medical attention and gradually resolve over time. However, if these side effects persist longer, please consult your doctor.
If you are known to be allergic to Espin TM Tablet or any other medicines, please inform your doctor. Pregnant or breastfeeding women should discontinue this Espin TM Tablet because it can cause injury and death to the developing fetus. Please do not stop taking Espin TM Tablet on your own, which may lead to the recurrence of symptoms or worsen the condition. Rise slowly if you have been sitting or lying down, as it may cause you to feel lightheaded or weak, especially when you stand up. Avoid potassium supplements with Espin TM Tablet as it may lead to high potassium levels in the blood. It is advised to drive with caution after taking Espin TM Tablet as it usually causes drowsiness and affects the driving ability.
Uses of Espin TM Tablet
Espin TM Tablet is used in the treatment of Hypertension (high blood pressure). The detailed use of Espin TM Tablet is as follows:
- Hypertension Management: Espin TM Tablet is primarily prescribed to lower high blood pressure, reducing the risk of heart-related complications.

Have a query?
Directions for Use
- Espin TM Tablet can be taken with or without food as advised by your doctor.
- Follow your doctor's instructions on the dosage and timing of this medication to ensure safety.
- Swallow Espin TM Tablet as a whole with a glass of water.
- Do not chew, crush or break it.
Medicinal Benefits
Espin TM Tablet is a combination of two medicines, namely, S-amlodipine and Telmisartan, primarily taken to prevent hypertension (high blood pressure). S-amlodipine belongs to a group of drugs called calcium channel blocker that dilates (widen) blood vessels and increase blood flow. S-amlodipine is equally effective at a half dose with better tolerability, and lesser side effects, including peripheral oedema, than amlodipine. Telmisartan is an angiotensin receptor blocker (ARB) that lowers increased blood pressure by blocking a naturally occurring substance known as angiotensin II (that tightens your blood vessels). It allows these constricted blood vessels to relax and, therefore, helps lower high blood pressure. It is used to lower the chances of stroke, heart attack and death. Collectively, Espin TM Tablet helps to lower high blood pressure, chest pain (angina), and other conditions caused by coronary artery disease.
How Espin TM Tablet Works
Storage
- Inform your doctor about the symptoms you're experiencing due to medication.
- Your doctor may adjust your treatment plan, which could include changing your medication, adding new medications, or offering advice on managing your symptoms.
- Practice good hygiene, including frequent handwashing, avoiding close contact with others, and avoiding sharing utensils or personal items.
- Stay hydrated by drinking plenty of fluids to help loosen and clear mucus from your nose, throat, and airways.
- Get plenty of rest and engage in stress-reducing activities to help your body recover. If your symptoms don't subside or worsen, consult your doctor for further guidance.
- Talk to your doctor about your back pain and potential medication substitutes or dose changes.
- Try yoga or Pilates and other mild stretching exercises to increase flexibility and strengthen your back muscles.
- To lessen the tension on your back, sit and stand upright and maintain proper posture.
- To alleviate discomfort and minimize inflammation, apply heat or cold packs to the afflicted area.
- Under your doctor's supervision, think about taking over-the-counter painkillers like acetaminophen or ibuprofen.
- Make ergonomic adjustments to your workspace and daily activities to reduce strain on your back.
- To handle tension that could make back pain worse, try stress-reduction methods like deep breathing or meditation.
- Use pillows and a supportive mattress to keep your spine in the right posture as you sleep.
- Back discomfort can worsen by bending, twisting, and heavy lifting.
- Speak with a physical therapist to create a customized training regimen to increase back strength and flexibility.
- Inform Your Doctor: Notify your doctor immediately about your diarrhoea symptoms. This allows them to adjust your medication or provide guidance on managing side effects.
- Stay Hydrated: Drink plenty of fluids to replace lost water and electrolytes. Choose water, clear broth, and electrolyte-rich drinks. Avoid carbonated or caffeinated beverages to effectively rehydrate your body.
- Follow a Bland Diet: Eat easy-to-digest foods to help firm up your stool and settle your stomach. Try incorporating bananas, rice, applesauce, toast, plain crackers, and boiled vegetables into your diet.
- Avoid Trigger Foods: Steer clear of foods that can worsen diarrhoea, such as spicy, fatty, or greasy foods, high-fibre foods, and dairy products (especially if you're lactose intolerant).
- Practice Good Hygiene: Maintain good hygiene to prevent the spread of infection. To stay healthy, wash your hands frequently, clean and disinfect surfaces regularly, and avoid exchanging personal belongings with others.
- Take Anti-Diarrheal Medications: If your doctor advises, anti-diarrheal medications such as loperamide might help manage diarrhoea symptoms. Always follow your doctor's directions.
- Keep track of your diarrhoea symptoms. If they don't get better or worse or are accompanied by severe stomach pain, blood, or dehydration signs (like extreme thirst or dark urine), seek medical help.
- Report to Your Doctor: Inform your doctor about the muscle pain, as they may need to adjust your medication.
- Stretch Regularly: Gentle stretching can help relieve muscle pain and stiffness.
- Stay Hydrated: Adequate water intake supports muscle health by removing harmful substances and maintaining proper muscle function.
- Warm or Cold Compresses: Apply cold or warm compresses to the affected area to reduce pain and inflammation.
- Rest and Relaxation: Adequate rest helps alleviate muscle strain, while relaxation techniques like deep breathing and meditation can soothe muscle tightness, calm the mind, and promote relief from discomfort.
- Gentle Exercise: Participate in low-impact activities, such as yoga or short walks, to improve flexibility, reduce muscle tension, and alleviate discomfort.
- Consult a physician: If your symptoms don't improve or get worse, go to the doctor for help and guidance.
- Consult your doctor if you experience symptoms of sinusitis, such as nasal congestion, facial pain, or headaches, which may be triggered by your medication.
- Your doctor may adjust your treatment plan by changing your medication, adding new medications, or providing guidance on managing your sinusitis symptoms.
- Practice good hygiene, including frequent handwashing, avoiding close contact with others, and avoiding sharing utensils or personal items.
- If your doctor advises, you can use nasal decongestants or saline nasal sprays to help relieve nasal congestion and sinus pressure.
- To help your body recover, get plenty of rest, stay hydrated, and engage in stress-reducing activities. If your symptoms persist or worsen, consult your doctor for further guidance.
- Please inform your doctor about joint pain symptoms, as they may adjust your medication regimen or prescribe additional medications to manage symptoms.
- Your doctor may prescribe common pain relievers if necessary to treat joint discomfort.
- Maintaining a healthy lifestyle is key to relieving joint discomfort. Regular exercise, such as low-impact sports like walking, cycling, or swimming, should be combined with a well-balanced diet. Aim for 7-8 hours of sleep per night to assist your body in repairing and rebuilding tissue.
- Applying heat or cold packs to the affected joint can help reduce pain and inflammation.
- Please track when joint pain occurs and any factors that may trigger it, and share this information with your doctor to help manage symptoms.
- If your joint pain is severe or prolonged, consult a doctor to rule out any underlying disorders that may require treatment.
- Prepare for a restful night's sleep: Develop a calming pre-sleep routine, like reading or meditation, to help your body relax and prepare for sleep.
- Create a sleep-conducive Environment: Make bedroom a sleep haven by ensuring it is quiet, dark and calm.
- Follow a Sleep Schedule: Go to bed and get up at the same time every day to help regulate your body's internal clock and increase sleep quality.
- Try relaxing techniques like deep breathing, mindfulness meditation and any others.
- Limit stimulating activities before bedtime: Avoid stimulating activities before bedtime to improve sleep quality.
- Monitor Progress: Keep track of your sleep patterns to identify areas for improvement.
- Consult a doctor if needed: If these steps don't improve your sleep, consult a doctor for further guidance and therapy.
What if I have taken an overdose of Espin TM Tablet
Drug Warnings
Don't stop taking Espin TM Tablet without talking to your doctor first. Stopping Espin TM Tablet abruptly may cause changes in your blood pressure and heart rhythm, cause chest pain or a heart attack. Your doctor will lower your dose gradually over a period of time to help prevent these symptoms. Espin TM Tablet should not be given to the people allergic to Espin TM Tablet or any of its ingredients, have low blood pressure (less than 90 mm of Hg), have had a heart attack, kidney disease, liver disease. Do not take Espin TM Tablet if you are pregnant, planning to conceive, or breastfeeding. Espin TM Tablet is not recommended to children below 18 years. Espin TM Tablet can cause ankle or foot swelling, raise your legs while you are sitting down and talk to your doctor if it does not go away. Avoid potassium supplements with Espin TM Tablet as it may lead to high potassium levels in the blood. Do not consume alcohol with Espin TM Tablet as it may increase the risk of low blood pressure.
Drug-Drug Interactions
Drug-Drug Interactions
Login/Sign Up
Co-administration of Aliskiren with Espin TM Tablet can increase the risk of hyperkalemia (high potassium levels in the blood).
How to manage the interaction:
Taking Espin TM Tablet with Aliskiren can possibly lead to an interaction, please consult a doctor before taking it. Do not discontinue the medications without consulting a doctor.
Taking Potassium Iodide with Espin TM Tablet can make high levels of potassium in the blood more likely.
How to manage the interaction:
Although taking Potassium iodide and Espin TM Tablet together can evidently cause an interaction, it can be taken if your doctor has suggested it. Do not stop using any medications without a doctor's advice.
Taking ramipril with Espin TM Tablet may increase the risk of side effects such as low blood pressure, kidney function impairment, and high blood potassium.
How to manage the interaction:
Although there is a possible interaction, Espin TM Tablet can be taken with ramipril if prescribed by the doctor. Consult the prescriber if you experience symptoms of high potassium such as nausea, vomiting, weakness, confusion, tingling of the hands and feet, feelings of heaviness in the legs, a weak pulse, or a slow or irregular heartbeat. Maintain adequate fluid intake during treatment with these medications. Do not discontinue the medications without consulting a doctor.
Taking tizanidine with Espin TM Tablet may have additive effects in lowering the blood pressure.
How to manage the interaction:
Although there is a possible interaction, Espin TM Tablet can be taken with tizanidine if prescribed by your doctor. Consult the prescriber if you experience symptoms of low blood pressure, such as headache, dizziness, lightheadedness, fainting, and/or changes in pulse or heart rate. Be cautious when getting up from a sitting or lying position. Do not discontinue the medications without consulting a doctor.
Taking trimethoprim with Espin TM Tablet may increase potassium levels in the blood.
How to manage the interaction:
Although there is an interaction between Espin TM Tablet and trimethoprim, they can be taken together if prescribed by a doctor. However, consult a doctor if you experience nausea, vomiting, weakness, confusion, tingling of the hands and feet, feelings of heaviness in the legs, and a weak pulse. Do not discontinue the medications without consulting a doctor.
Co-administration of amiloride with Espin TM Tablet may increase potassium levels in the blood. (High potassium levels can cause hyperkalemia, which can lead to kidney failure, muscular paralysis, abnormal heart rhythm).
How to manage the interaction:
Although there is a possible interaction, amiloride may lead to an interaction but can be taken if prescribed by the doctor. However, consult the doctor if you experience nausea, vomiting, weakness, disorientation, tingling in your hands and feet, feelings of heaviness in your legs, a weak pulse, or a slow or irregular heartbeat. It is important to maintain proper fluid intake while taking these medications. Do not stop using any medications without talking to a doctor.
Taking lisinopril with Espin TM Tablet may increase the levels of potassium in blood.
How to manage the interaction:
Although there is a possible interaction, Espin TM Tablet can be taken with lisinopril if prescribed by the doctor. Consult the prescriber if you experience symptoms of high potassium such as nausea, vomiting, weakness, confusion, tingling of the hands and feet, feelings of heaviness in the legs, a weak pulse, or a slow or irregular heartbeat. Maintain adequate fluid intake during treatment with these medications.
Co-administration of Espin TM Tablet may significantly increase the blood levels of lithium.
How to manage the interaction:
Although there is a possible interaction, Espin TM Tablet can be taken with lithium if prescribed by the doctor. Consult the prescriber if you experience symptoms of lithium intoxication such as drowsiness, dizziness, confusion, loose stools, vomiting, muscle weakness, muscle incoordination, shaking of hands and legs, blurred vision, ringing in the ear, excessive thirst, or increased urination. Do not discontinue the medication without consulting a doctor.
Co-administration of Espin TM Tablet increases levels of eluxadoline by increasing metabolism.
How to manage the interaction:
Taking Espin TM Tablet with Eluxadoline together can possibly result in an interaction, but it can be taken if your doctor has advised it. Do not discontinue any medications without consulting a doctor.
Taking perindopril with Espin TM Tablet may increase the risk of side effects such as low blood pressure, kidney function impairment, and high blood potassium.
How to manage the interaction:
Although there is a possible interaction, Espin TM Tablet can be taken with perindopril if prescribed by the doctor. Consult the prescriber if you experience symptoms of high potassium such as nausea, vomiting, weakness, confusion, tingling of the hands and feet, feelings of heaviness in the legs, a weak pulse, or a slow or irregular heartbeat. Maintain adequate fluid intake during treatment with these medications. Do not discontinue the medications without consulting a doctor.
Drug-Food Interactions
Drug-Food Interactions
Login/Sign Up
Lentils, Orange Juice, Oranges, Raisins, Potatoes, Salmon Dried, Spinach, Tomatoes, Sweet Potatoes, Coconut Water, Beans, Beetroot, Broccoli, Bananas, Apricots, Avocado, Yogurt
How to manage the interaction:
Consuming high potassium-containing foods while taking S-amlodipine and telmisartan can cause high levels of potassium in the blood, increasing the risk of side effects such as weakness, an irregular heartbeat, confusion, or feelings of heaviness in the legs. Limit or avoid high potassium-containing foods when using S-amlodipine and telmisartan, as they may cause an interaction.
Diet & Lifestyle Advise
Keep your weight under control with BMI 19.5-24.9.
- Do regular physical activity or exercise for at least 150 minutes per week or about 30 minutes most days of the week. Doing this can help you to lower your raised blood pressure by about 5 mm of Hg.
- Limit intake of sodium chloride (table salt) in your daily diet to 2300 mg per day or less than 1500 mg is ideal for most adults.
- If you are taking alcohol, then only one serving for women and two servings for men is advisable.
- Quitting smoking is the best strategy to lower the risk of heart disease.
- Avoid chronic stress as it can raise your blood pressure. Try to enjoy and spent time with your loved ones to cope with stress and practice mindfulness techniques.
- Monitor your blood pressure daily and if there is too much fluctuation, then immediately contact your doctor.
- Try to include heart-healthy omega 3 fatty acids containing food drinks in your daily diet. You can also use low-fat cooking oil like olive oil, soybean oil, canola oil and coconut oil to lower your elevated blood pressure.
Habit Forming
Therapeutic Class
All Substitutes & Brand Comparisons
RX
Esloza-TM Tablet 10's
Medinza Biotech
₹45
(₹4.05 per unit)
66% CHEAPERRX
Numlo-TM 2.5 mg Tablet 15's
Emcure Pharmaceuticals Ltd
₹236
(₹14.16 per unit)
18% COSTLIERRX
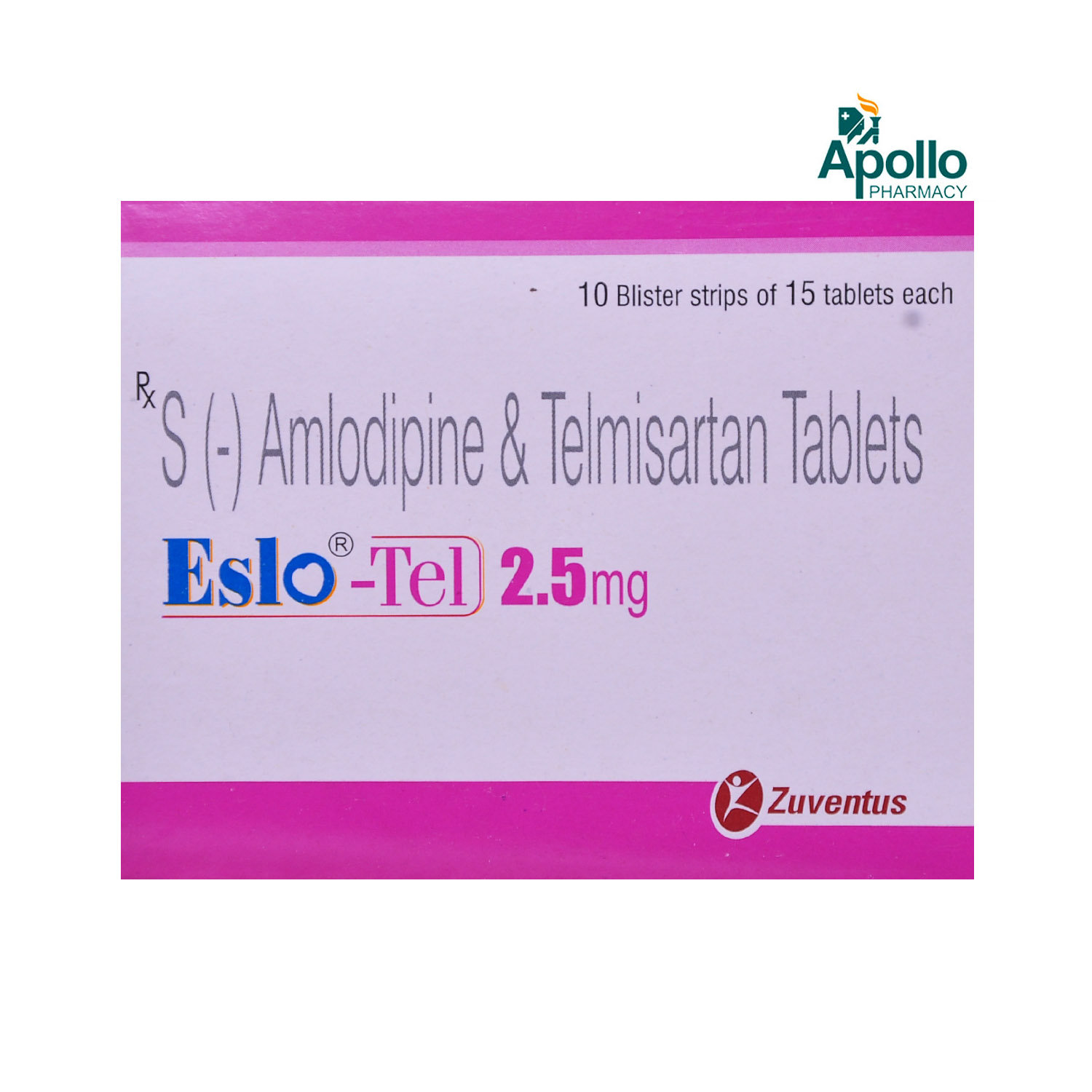
Eslo-Tel 2.5 mg Tablet 15's
Zuventus Healthcare Ltd
₹257
(₹15.42 per unit)
28% COSTLIER
Alcohol
Unsafe
Espin TM Tablet and alcohol together result in an abnormal decrease in blood pressure levels, thus strictly not to be taken together.
Pregnancy
Unsafe
Espin TM Tablet is not recommended and unsafe in pregnancy. It can affect and harm the baby. Consult your doctor before taking Espin TM Tablet if you plan to become pregnant or already pregnant. Your doctor will weigh the potential risks and benefits before prescribing Espin TM Tablet .
Breast Feeding
Unsafe
Espin TM Tablet is known to pass breast milk, but its effect on the baby is not known. So, before breastfeeding, let your doctor know about this. Either you need to stop breastfeeding for using Espin TM Tablet or stop taking Espin TM Tablet .
Driving
Caution
Espin TM Tablet may cause side effects like dizziness, headaches, nausea, or tiredness, which can affect your ability to concentrate and drive. Hence, it is recommended not to drive or operate machinery until you are mentally alert.
Liver
Caution
Espin TM Tablet has been found to affect liver function in certain cases thus patients with liver problems should discuss with their doctor for proper guidance regarding treatment with this medication.
Kidney
Caution
Espin TM Tablet consists of Telmisartan drug, which may affect the kidney functioning. A patient is strictly advised to consult and discuss with his/her doctor before taking this medication.
Children
Unsafe
Espin TM Tablet is not recommended for use in the people below 18 years of age as its safety and effectiveness have been not established.
Heart
Safe if prescribed
Espin TM Tablet is safe for use in heart patients if recommended by the physician.
Geriatrics
Caution
Espin TM Tablet should be used under caution in geriatric patients. Please consult your physician.
FAQs
Espin TM Tablet belongs to the class of medicines called anti-hypertensives used to treat hypertension (high blood pressure).
Espin TM Tablet is a combination of two medicines: S-Amlodipine and Telmisartan. S-Amlodipine is a calcium channel blocker (CCB) and Telmisartan is an angiotensin receptor blocker (ARB). They work by relaxing the blood vessels and making the heart more efficient at pumping blood throughout the body. Together, they lower blood pressure effectively.
Espin TM Tablet not recommended to take if you are pregnant as it can cause damage to the unborn baby (may lead to fetal toxicity). It contains telmisartan, a category D pregnancy drug and it is harmful to the baby.
No, you are advised to inform your doctor and monitor your blood pressure for at least two weeks before stopping the medicine. Depending upon your current blood pressure readings, there is a possibility your doctor may lower your medicine dosage and not recommend discontinuing it.
Espin TM Tablet contains telmisartan which may increase potassium levels in the blood (hyperkalemia). Therefore, it is recommended to avoid the intake of potassium supplements and foods that are rich in potassium like coconut water, bananas and broccoli.
Yes, Espin TM Tablet contains S-amlodipine, which is known to cause ankle swelling upon long term use. Please try to keep your feet up when sitting for long hours. If the problem persists still, consult your doctor and do as advised.
Please inform your doctor before surgery if you are taking Espin TM Tablet as it needs to be stopped because it might lower the blood pressure further if taken along with general anesthesia.
Espin TM Tablet can be taken at any time of the day, with or without food. But try to take it at the same time each day to see the best results. However, based on your age, body weight, and medical condition, your doctor will determine when it is appropriate for you to take Espin TM Tablet .
The common side effects of Espin TM Tablet are dizziness, stomach pain, nausea, constipation, double vision, muscle cramps, swollen ankles, oedema (fluid retention), and hypotension (low blood pressure). If any of these side effects persist or worsen, please consult your doctor.
If you stop taking Espin TM Tablet , your blood pressure may increase, and your condition may worsen. Consult your doctor before stopping or changing your treatment plan to ensure your blood pressure remains controlled.
If you forget to take a dose of Espin TM Tablet , take it as soon as you remember. However, if it is almost time for your next dose, skip the missed dose and continue with your regular dosing schedule. Do not double the dose to make up the dose.
Take Espin TM Tablet at the same time every day to help you remember to take it. Monitor your blood pressure regularly to ensure the medication is working effectively. Before taking Espin TM Tablet , inform your doctor if you have any pre-existing medical conditions. Avoid consuming alcohol as it can worsen dizziness. Stop taking Espin TM Tablet and consult your doctor immediately if you become pregnant. Regularly visit your doctor and take all the necessary blood tests your doctor recommends without fail.
It is advised to avoid consuming alcohol while taking Espin TM Tablet . Alcohol can raise blood pressure and may increase the risk of side effects like dizziness and drowsiness.
Taking more than the required dose of Espin TM Tablet leads to an overdose. Symptoms of overdose include low blood pressure, abnormal heartbeat, fainting, drowsiness, nausea, vomiting or confusion. If you experience these symptoms or suspect you have taken an overdose, seek immediate medical attention, even if there are no symptoms.
Take Espin TM Tablet as prescribed by your doctor. Typically, Espin TM Tablet can be taken daily to manage high blood pressure. Therefore, please consult your doctor before using Espin TM Tablet ; your doctor will evaluate your health condition and suggest whether you can take Espin TM Tablet every day.
Espin TM Tablet may alter the blood sugar levels in your body. Therefore, please inform your doctor if you have diabetes before taking Espin TM Tablet . Your doctor will closely monitor your blood sugar levels to avoid the risk of side effects.
Country of origin
Manufacturer/Marketer address
Customers Also Bought
Disclaimer
Author Details
We provide you with authentic, trustworthy and relevant information
Reference
- https://www.medicines.org.uk/emc/files/pil.6068.pdf
- https://www.medicines.org.uk/emc/files/pil.3166.pdf
- https://downloads.hindawi.com/journals/ijhy/2018/8681792.pdf
- https://www.sanofi.in/-/media/Project/One-Sanofi-Web/Websites/Asia-Pacific/Sanofi-IN/Home/science-and-innovation/for-healthcare-professionals/product-information/Telsite-am-PI-June-2018.pdf?
Buy best Cardiology products by
Torrent Pharmaceuticals Ltd
Sun Pharmaceutical Industries Ltd
Lupin Ltd
Intas Pharmaceuticals Ltd
Cipla Ltd
Micro Labs Ltd
Macleods Pharmaceuticals Ltd
Abbott India Ltd
Ajanta Pharma Ltd
Ipca Laboratories Ltd
Eris Life Sciences Ltd
Mankind Pharma Pvt Ltd
Lloyd Healthcare Pvt Ltd
Dr Reddy's Laboratories Ltd
Emcure Pharmaceuticals Ltd
Alembic Pharmaceuticals Ltd
Glenmark Pharmaceuticals Ltd
Alkem Laboratories Ltd
Zydus Healthcare Ltd
East West Pharma India Pvt Ltd
USV Pvt Ltd
Aristo Pharmaceuticals Pvt Ltd
Alteus Biogenics Pvt Ltd
J B Chemicals & Pharmaceuticals Ltd
Elbrit Life Sciences Pvt Ltd
Fusion Health Care Pvt Ltd
Eswar Therapeutics Pvt Ltd
La Renon Healthcare Pvt Ltd
Zydus Cadila
Akumentis Healthcare Ltd
Hbc Life Sciences Pvt Ltd
Troikaa Pharmaceuticals Ltd
Knoll Healthcare Pvt Ltd
Corona Remedies Pvt Ltd
Morepen Laboratories Ltd
Shrrishti Health Care Products Pvt Ltd
Prevego Healthcare & Research Pvt Ltd
Lividus Pharmaceuticals Pvt Ltd
Medley Pharmaceuticals Ltd
Cadila Pharmaceuticals Ltd
Jubilant Lifesciences Ltd
Msn Laboratories Pvt Ltd
Zuventus Healthcare Ltd
Steris Healthcare
Ranmarc Labs
Elder Pharmaceuticals Ltd
Tas Med India Pvt Ltd
Unison Pharmaceuticals Pvt Ltd
Primus Remedies Pvt Ltd
Leeford Healthcare Ltd
Blue Cross Laboratories Pvt Ltd
Azkka Pharmaceuticals Pvt Ltd
Sanofi India Ltd
Sinsan Pharmaceuticals Pvt Ltd
Nirvana India Pvt Ltd
Knoll Pharmaceuticals Ltd
Orsim Pharma
Systopic Laboratories Pvt Ltd
Indiabulls Pharmaceuticals Pvt Ltd
RPG Life Sciences Ltd
Biochem Pharmaceutical Industries Ltd
Johnlee Pharmaceuticals Pvt Ltd
Olcare Laboratories Pvt Ltd
Vasu Organics Pvt Ltd
Cadila Healthcare Ltd
Econ Healthcare
Shine Pharmaceuticals Ltd
Xemex Life Sciences
Elicad Pharmaceuticals Pvt Ltd
Elinor Pharmaceuticals (P) Ltd
Sunij Pharma Pvt Ltd
Orris Pharmaceuticals
Atos Lifesciences Pvt Ltd
FDC Ltd
Lia Life Sciences Pvt Ltd
Pfizer Ltd
MEDICAMEN BIOTECH LTD
Nicholas Piramal India Ltd
Astra Zeneca Pharma India Ltd
Lakshya Life Sciences Pvt Ltd
Opsis Care Lifesciences Pvt Ltd
Alvio Pharmaceuticals Pvt Ltd
Biocon Ltd
Finecure Pharmaceuticals Ltd
Glynis Pharmaceuticals Pvt Ltd
Indoco Remedies Ltd
Med Manor Organics Pvt Ltd
Acmedix Pharma Llp
Allysia Lifesciences Pvt Ltd
Chemo Healthcare Pvt Ltd
Pficus De Med Pvt Ltd
Proqol Health Care Pvt Ltd
Divine Savior Pvt Ltd
Enovus Healthcare Pvt Ltd
Ergos Life Sciences Pvt Ltd
Samarth Life Sciences Pvt Ltd
Signova Pharma
ALICAN PHARMACEUTICAL PVT LTD
Auspharma Pvt Ltd
Maxford Labs Pvt Ltd
Recommended for a 30-day course: 3 Strips